
Table of Contents:
- Introduction to Personalized Medicine
- The Science Behind Personalized Medicine
- Genomics and Genetics
- Proteomics and Metabolomics
- Biomarkers in Personalized Medicine
- How Personalized Medicine Differs from Traditional Medicine
- Key Components and Technologies Driving Personalized Medicine
- Artificial Intelligence and Machine Learning
- Big Data Analytics in Healthcare
- Next-Generation Sequencing (NGS)
- CRISPR and Gene Editing
- Personalized Medicine in Cancer Treatment
- Precision Oncology
- Targeted Therapies
- Immunotherapies
- Personalized Medicine in Other Disease Areas
- Cardiovascular Diseases
- Neurological Disorders
- Rare Genetic Diseases
- Pharmacogenomics: Tailoring Drug Therapy
- The Role of Genetics in Drug Response
- Case Studies in Pharmacogenomics
- Benefits of Personalized Medicine for Patients and Healthcare Providers
- Improved Patient Outcomes
- Cost-Effectiveness
- Preventive Care and Early Diagnosis
- The Ethical, Legal, and Social Implications of Personalized Medicine
- Data Privacy and Security
- Access and Equity
- The Role of Informed Consent
- Personalized Medicine and Patient Empowerment
- How Personalized Medicine Involves Patients in Their Own Care
- The Role of Patient Advocacy
- Future Prospects: What’s Next for Personalized Medicine?
- Emerging Technologies and Innovations
- Precision Health: Moving Beyond Treatment to Prevention
- Challenges and Barriers in Implementing Personalized Medicine
- Healthcare System Barriers
- Cost and Reimbursement Issues
- Integrating Personalized Medicine into Everyday Clinical Practice
- Conclusion: The Transformative Power of Personalized Medicine
Introduction to Personalized Medicine
Personalized medicine represents a groundbreaking approach to healthcare, where medical decisions, treatments, and practices are tailored to the individual patient based on their genetic makeup, lifestyle, and environment. This shift from a “one-size-fits-all” model to one that considers the unique biological factors of each patient is reshaping how we approach disease prevention, diagnosis, and treatment.
Personalized medicine aims to predict which medical treatments will be most effective for each patient, minimizing adverse reactions and maximizing positive outcomes. Advances in fields such as genomics, proteomics, and bioinformatics are enabling this transformation, offering new opportunities for tailored therapies that target specific diseases at a molecular level.
The Science Behind Personalized Medicine
Genomics and Genetics The cornerstone of personalized medicine lies in our understanding of genetics. Human beings share approximately 99.9% of their DNA, but it is the remaining 0.1% that accounts for variations in disease susceptibility, drug response, and other health-related factors. By studying a patient’s genome, doctors can identify genetic variants that may contribute to the risk of developing certain conditions or influence how an individual might respond to a particular drug.
Proteomics and Metabolomics Beyond genomics, the study of proteins (proteomics) and metabolites (metabolomics) also plays a critical role in personalized medicine. Proteins are the functional molecules in the body that drive biological processes, and understanding their structure and function is crucial for identifying disease biomarkers. Metabolomics focuses on the unique chemical fingerprints left behind by cellular processes, providing insights into the dynamic biochemical changes within the body.
Biomarkers in Personalized Medicine Biomarkers are biological molecules that indicate the presence of a disease or the response of the body to treatment. They are essential tools in personalized medicine, offering physicians valuable insights into disease progression and patient response to therapies. Biomarkers can be genetic, proteomic, or metabolomic in nature, and their discovery has been critical in the development of personalized treatments.
How Personalized Medicine Differs from Traditional Medicine
Traditional medicine often employs a generalized treatment approach, where patients with similar symptoms receive similar treatments. However, not all patients respond to the same treatment in the same way, leading to varying outcomes. Personalized medicine, on the other hand, uses detailed patient data to tailor medical care to each individual, improving the effectiveness of treatments and minimizing side effects.
In traditional medicine, therapies are developed and tested based on population averages, which may not always apply to individual patients. Personalized medicine focuses on the individual, using predictive tools to assess the likelihood of success for a particular treatment, and sometimes even developing customized therapies based on the patient’s unique profile.
Key Components and Technologies Driving Personalized Medicine
Artificial Intelligence and Machine Learning AI and machine learning are revolutionizing the field of personalized medicine by enabling the analysis of vast datasets, including genomic information, electronic health records, and real-time patient data. These technologies help identify patterns and correlations that might not be visible through traditional methods, accelerating the discovery of new treatment options.
Big Data Analytics in Healthcare The volume of healthcare data generated today is staggering, and big data analytics plays a crucial role in harnessing this information for personalized medicine. By analyzing large-scale datasets from diverse patient populations, researchers can identify trends, predict outcomes, and develop more effective treatment strategies tailored to individual patients.
Next-Generation Sequencing (NGS) Next-generation sequencing (NGS) has dramatically reduced the cost and time required for genomic sequencing, making it a critical tool in personalized medicine. NGS allows for the rapid analysis of a patient’s entire genome, enabling the identification of genetic mutations or variants that may impact disease risk or treatment response.
CRISPR and Gene Editing The CRISPR-Cas9 gene-editing technology has opened up new possibilities in personalized medicine by enabling the precise modification of genetic material. With CRISPR, scientists can target and edit specific genes that contribute to disease, potentially offering cures for genetic disorders. While the use of CRISPR in clinical settings is still in its early stages, it holds tremendous promise for personalized therapies.
Personalized Medicine in Cancer Treatment
Precision Oncology Cancer treatment has been one of the biggest beneficiaries of personalized medicine. Precision oncology tailors cancer treatments based on the genetic makeup of an individual’s tumor, allowing for the selection of therapies that are more likely to be effective. Advances in cancer genomics have led to the development of targeted therapies that attack cancer cells while sparing healthy ones.
Targeted Therapies Targeted cancer therapies focus on specific molecules within cancer cells that drive tumor growth. By targeting these molecules, these therapies can more effectively kill cancer cells while reducing damage to surrounding healthy tissue. Personalized medicine has made it possible to match patients with the targeted therapies that are most likely to work based on the genetic characteristics of their tumor.
Immunotherapies Immunotherapy has become a promising avenue in cancer treatment, harnessing the patient’s immune system to fight the disease. Personalized immunotherapies, such as CAR-T cell therapy, are designed to recognize and attack cancer cells with precision, offering new hope for patients with certain types of cancer.
Personalized Medicine in Other Disease Areas
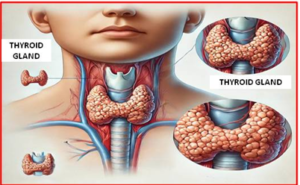
Cardiovascular Diseases Personalized medicine is making strides in cardiovascular care by identifying genetic factors that influence heart disease risk and treatment response. For example, pharmacogenomic testing can help determine how patients with cardiovascular conditions will respond to blood thinners or cholesterol-lowering medications, allowing for more precise dosing and better outcomes.
Neurological Disorders Neurological conditions, such as Alzheimer’s disease and Parkinson’s disease, have complex genetic and environmental causes. Personalized medicine is helping researchers identify biomarkers that can predict the risk of developing these conditions, enabling earlier intervention and more effective treatments.
Rare Genetic Diseases For patients with rare genetic diseases, personalized medicine offers new hope through therapies that target the underlying genetic cause of their condition. Advances in gene therapy and gene editing have made it possible to develop treatments that address the root cause of rare diseases, improving quality of life for patients.
Pharmacogenomics: Tailoring Drug Therapy
The Role of Genetics in Drug Response Pharmacogenomics studies how an individual’s genetic makeup influences their response to drugs. Variations in certain genes can affect how a person metabolizes medications, leading to differences in drug efficacy and the likelihood of side effects. By understanding a patient’s genetic profile, doctors can select the right drug and dosage for optimal results.
Case Studies in Pharmacogenomics Several case studies have demonstrated the potential of pharmacogenomics to improve patient outcomes. For example, patients with certain genetic mutations may metabolize common painkillers, like codeine, too quickly or too slowly, leading to dangerous side effects or inadequate pain relief. Pharmacogenomic testing can guide physicians in selecting the safest and most effective pain management strategies.
Benefits of Personalized Medicine for Patients and Healthcare Providers
Improved Patient Outcomes By tailoring treatments to the individual patient, personalized medicine can significantly improve outcomes. Patients are more likely to receive treatments that work for them, reducing the trial-and-error approach often seen in traditional medicine.
Cost-Effectiveness Although personalized medicine involves advanced testing and data analysis, it has the potential to reduce healthcare costs in the long run. By selecting the most effective treatments from the start, patients can avoid costly complications and hospitalizations associated with ineffective therapies.
Preventive Care and Early Diagnosis Personalized medicine also emphasizes prevention, using genetic testing and biomarkers to identify individuals at high risk for certain conditions. By intervening early, doctors can prevent diseases from developing or progressing, leading to better health outcomes and reduced healthcare costs.



1 thought on “Revolutionizing Healthcare: The Rise of Personalized Medicine”
I found your discussion on sleep hygiene really helpful. I’ve been struggling with sleep lately, and I’ll implement some of these tips.