INTRODUCTION
A healthy diet during pregnancy is essential for the well-being of both the mother and the developing baby. The right nutrients support the baby’s growth, development, and overall health while also helping the mother maintain her energy, manage changes, and prepare for childbirth. Pregnancy places additional demands on the body, making it crucial to focus on specific nutrients that are required in higher amounts during this time. During pregnancy, a woman’s body goes through various physiological transformations that help the fetus grow and also prepare both for labor and delivery. (1,2)
Certain nutrients play a particularly important role in a healthy pregnancy. For example, folic acid is vital in the early stages to reduce the risk of neural tube defects, while iron helps prevent anemia by supporting the increased blood volume. Calcium and vitamin D work together to support the development of the baby’s bones and teeth. Protein is essential for tissue growth, and omega-3 fatty acids support brain and eye development.
A pregnancy diet should also include an appropriate balance of carbohydrates, healthy fats, fiber, and vitamins and minerals to meet the growing nutritional needs. Eating a variety of nutrient-rich foods such as whole grains, lean proteins, fruits, vegetables, and dairy products ensures that both the mother and the baby receive the necessary nutrients.
Pregnant women should aim to maintain a balanced and nutrient-rich diet, minimizing the intake of unhealthy foods and prioritizing whole, unprocessed options. Working with a healthcare provider or nutritionist can help customize the diet to meet the unique needs of the pregnancy, promoting a safe and healthy journey for both the mother and the baby.
Essential nutrients required during pregnancy:
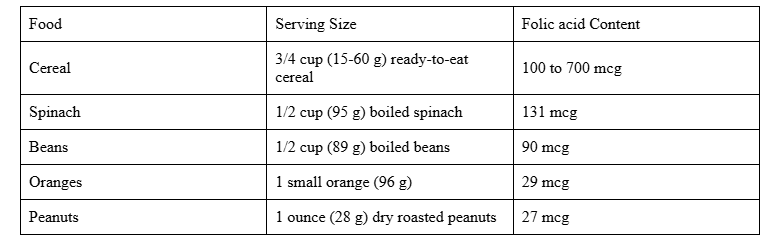
- Folic acid or Folate: Prevent brain and spinal cord birth problems
Folate, a type of B vitamin, plays a crucial role in preventing severe issues in the developing brain and spinal cord, such as neural tube defects. Its synthetic version, found in fortified foods and supplements, is called folic acid. Taking folic acid has been proven to reduce the chances of premature birth and low birth weight in babies.
Recommended Intake: Before conception, you need 400 micrograms (mcg) of folate or folic acid daily to support healthy development. During pregnancy, this requirement increases to 600–1,000 mcg per day to ensure proper growth and reduce the risk of neural tube defects in your baby.
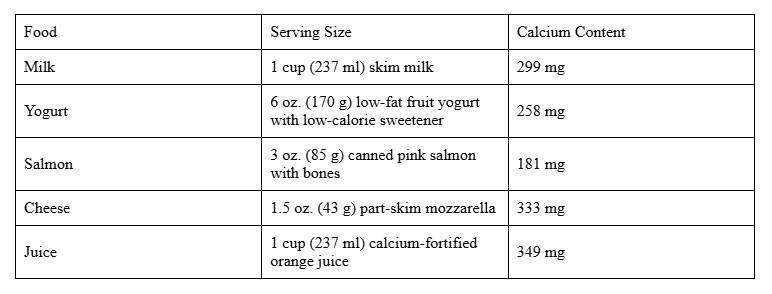
- Calcium: Strengthen bones
Both you and your baby require calcium to build and maintain strong bones and teeth. In addition to this, calcium is essential for the proper functioning of the circulatory, muscular, and nervous systems. It also plays a vital role in blood clotting, hormone release, and ensuring your baby’s overall healthy growth and development during pregnancy.
Recommended Intake: Pregnant women require 1,000 milligrams (mg) of calcium daily to support their baby’s bone and teeth development, while pregnant teenagers need a slightly higher intake of 1,300 mg per day to meet their growing bodies’ additional needs.
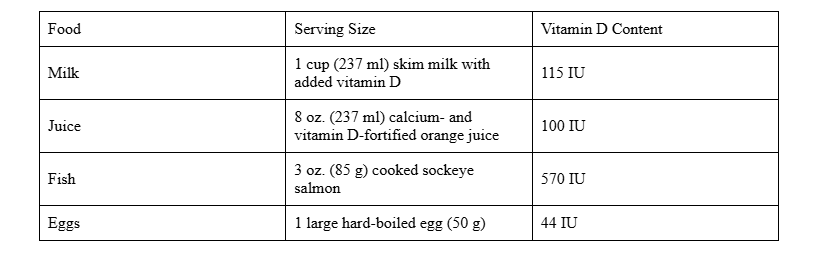
- Vitamin D: Promote bone strength
Vitamin D works hand in hand with calcium to support the formation of your baby’s strong bones and healthy teeth. It also plays a crucial role in helping the body absorb calcium effectively, promoting proper skeletal development and reducing the risk of bone-related issues for both you and your baby.
Recommended Intake: It is recommended to consume 600 international units (IU) of vitamin D daily during pregnancy to support your baby’s bone development and overall health, as well as to aid calcium absorption in your body.
- Protein: Promote growth
Protein is essential for your baby’s growth and development throughout pregnancy, as it supports the formation of new cells, tissues, and organs. It also plays a key role in building the placenta, ensuring proper nutrient transfer to your baby, and maintaining your own health during this critical time.
Recommended Intake: During pregnancy, you should aim to consume 71 grams (g) of protein daily. This helps support your baby’s growth, the development of tissues and organs, and the increased demands of your own body during this critical time.

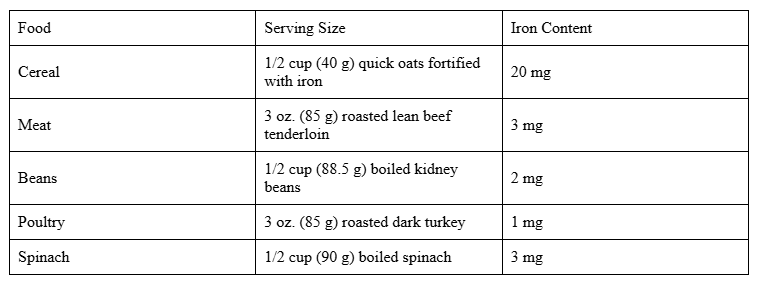
- Iron: Prevent iron deficiency anemia
Iron is essential for the production of hemoglobin, a protein in red blood cells responsible for carrying oxygen to the body’s tissues. During pregnancy, your body requires twice as much iron as usual to produce extra blood needed to supply oxygen to your growing baby.
If your iron levels are too low or your stores are insufficient, you may develop iron deficiency anemia. This can lead to symptoms such as fatigue, weakness, and headaches. Severe cases during pregnancy can increase the risk of complications, including premature birth, low birth weight, and postpartum depression.
Recommended Intake: During pregnancy, it is recommended to get 27 milligrams (mg) of iron daily. This helps support the increased blood volume needed to carry oxygen to both you and your baby, reducing the risk of iron deficiency anemia.
- Omega-3 fatty acids: Supports brain development
Omega-3 fatty acids are a type of healthy fat found naturally in several fish, such as salmon, mackerel, and sardines, and play a vital role in supporting brain development before and after birth. These essential fats are also important for reducing inflammation and promoting overall health. Flaxseed, whether ground or in oil form, is an excellent plant-based source of omega-3s. In addition, omega-3s can be found in a variety of other foods, including broccoli, cantaloupe, kidney beans, spinach, cauliflower, and walnuts, making it easier to include these healthy fats in your diet.
Recommended Intake: The recommended intake of omega-3 fatty acids during pregnancy is about 200-300 milligrams (mg) per day of DHA (a type of omega-3) to support the development of your baby’s brain and eyes.
For non-pregnant individuals, a general recommendation is 250-500 mg of combined EPA and DHA per day for overall health.

Weight Gain: What’s Normal?
If you’re worried about gaining weight during pregnancy, try not to stress. It’s completely natural to gain some weight, as it supports the baby’s nourishment. A portion of this weight is also stored to help with breastfeeding once the baby is born.
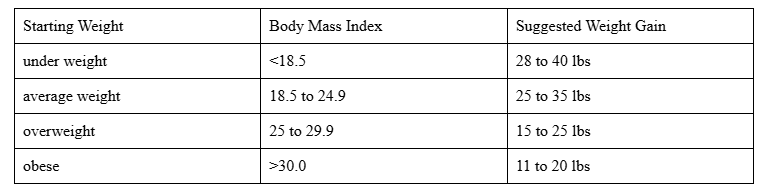
On average, women gain about 25 to 35 pounds during pregnancy. However, the amount of weight gained can vary. Women who are underweight before pregnancy may gain more, while those with higher pre-pregnancy weight may gain less.
Ideal Weight Gain during Pregnancy with One Baby:
What foods should be restricted during pregnancy?
- Alcohol: There is no known safe amount of alcohol to consume during pregnancy.
- Fish with high mercury levels: Limit white (albacore) tuna to 6 ounces per week, and avoid eating tilefish, shark, swordfish, marlin.
- Foods that could carry harmful germs: These include:
- Refrigerated smoked seafood, such as whitefish, and mackerel
- Undercooked meat, poultry, eggs, and seafood
- Refrigerated meat spreads
- Pre-made salads like chicken, egg, or tuna salad
- Unpasteurized or raw milk
- Unpasteurized juices or cider
- Soft cheeses made from unpasteurized milk
- Raw sprouts of any kind (such as alfalfa, clover, radish, and mung beans)
- Raw cookie dough
- Unwashed fruits and vegetables
- Excessive caffeine: Drinking too much caffeine may harm your baby. It’s recommended to limit caffeine under 200 mg per day during pregnancy.
GESTATIONAL DIABETES
Gestational diabetes is a condition characterized by high blood sugar that develops or is first detected during pregnancy. Women with gestational diabetes are more likely to give birth to larger babies, which can lead to complications during delivery.
The goals of Medical Nutrition Therapy (MNT) in Gestational Diabetes include:
- The meal plan should ensure sufficient calories and nutrients to meet both maternal and fetal needs in pregnancy.
- Caloric requirements vary based on factors such as age, activity level, pre-pregnancy weight, and the stage of pregnancy.
- During the second and third trimesters, an increase of 350 kcal above the baseline requirement, or approximately 30-40 kcal per kilogram of ideal body weight, is recommended.
Diet management plan for pregnant woman experiencing vomiting:
Vomiting leads to the loss of fluids and electrolytes in the body, so the primary focus should be on keeping the pregnant woman properly hydrated.
To achieve this:
- Drink fluids in small sips throughout the day, such as electrolyte drinks, lemonade, or diluted fruit juices.
- Consume snacks with high water content like watermelon, canned fruit, fruit juice bars, or flavored ice cubes.
- Easy-to-Digest Foods:
- Eat low-fat, bland foods like crackers, rice, toast, and boiled potatoes.
- Avoid spicy, greasy, or strong-smelling foods.
- Small, Frequent Meals:
- Have small meals every 2-3 hours to prevent nausea, like applesauce, plain yogurt, or oatmeal.
- Use Ginger and Vitamin B6:
- Try ginger in tea, candies, or ginger ale to help reduce nausea.
- Consider Vitamin B6 (with medical advice) for relief.
- Avoid Strong Odors: Steer clear of foods with strong smells to prevent triggering nausea.
During pregnancy, constipation is a common issue. To manage constipation during pregnancy, the following dietary changes can be helpful:
- Increase Fruit and Vegetable Intake: Eat plenty of fiber-rich fruits and vegetables to promote regular bowel movements.
- Stay Hydrated: Drink plenty of fluids throughout the day to help soften stool and prevent dehydration.
- Avoid Mineral Oils and Natural Remedies: Refrain from using mineral oils or other natural remedies, as they can have unwanted effects during pregnancy.
- Avoid Laxatives: Do not use laxatives, unless advised by a healthcare provider, as they may not be safe during pregnancy. (3)
REFERENCES
- Heidemann B.H., McClure J.H. Changes in maternal physiology during pregnancy. BJA CEPD Rev. 2003;3:65–68. doi: 10.1093/bjacepd/mkg065.
- Soma-Pillay P., Nelson-Piercy C., Tolppanen H., Mebazaa A. Physiological changes in pregnancy. Cardiovasc. J. Afr. 2016;27:89–94. doi: 10.5830/CVJA-2016-021.
- Seshiah et al. Gestational Diabetes Mellitus – Indian Guidelines. JAPI, Vol. 54 August, 2006.